What is an Achilles tendinopathy?
‘Tendinopathy ‘is described along a continuum that there is a continuum of tendon pathology that has three stages: reactive tendinopathy, tendon dysrepair (failed healing) and degenerative tendinopathy (read more into tendinopathy on article about tendinopathy).
Achilles tendinopathy is a condition resulting in posterior ankle pain. The word tendinopathy is used to describe a pathological change to the tendon which consists of microtears, degeneration of collagen fibres with replacement by scar tissue and premature death of tendon cells (tenocyte apoptosis). Tendinopathies develop along a continuum and depend on the conditioning of the individual, some may be through overload (either in athletes or deconditioned individualy who suddenly increase activitiy) or as a failed healing response of a tendon or due to chronic overload or compression of a degenerative tendon.
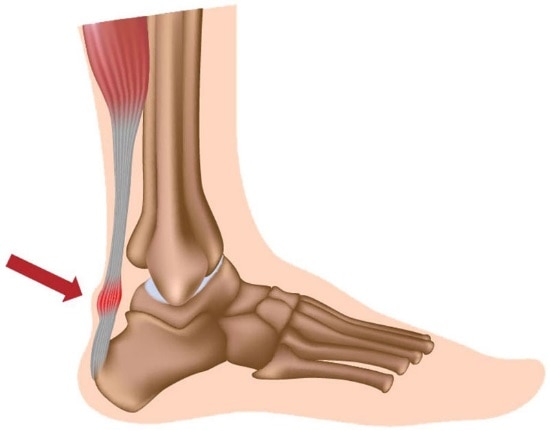
Achilles Tendon Anatomy
The Achilles tendon is one of the strongest tendons in our body. It is a thick band of fibrous connective tissue that connects the gastrocnemius and soleus (calf muscles) to the heel bone (calcaneum). The calf muscle, via the Achilles tendon, contracts and plantar flexed our foot, which points our toe towards the ground. When we dorsiflex our ankle (toes to the ceiling) the Achilles tendon is placed on stretch. It also has fibers that become part of the plantarfascia through myofascial connections.
What causes Achilles tendinopathies?
Achilles tendinopathies develop when the load they are placed under is greater than what the tendon can withstand and adapt to. While the pain may feel as if it had a sudden onset, tendinopathic changes occur over a sustained period of high training loads or a sudden increase in volume of training load. Hence most tendinopathies may develop several weeks after increasing training volume or taking up a new activity. Other contributing factors to Achilles tendinopathies may include unsupportive footwear, changes in training surface (hard or inclined surface) and a variety of biomechanical factors (see the end of this article).
As Achilles Tendinopathies are sometime classified as overload injuries, they are most common in running and jumping athletes. They are common in sports requiring explosive movements such as soccer, basketball, Australian rules football or netball where athletes are placing high demands on the Achilles tendon through plyometric movement.
Achilles tendinopathies are not just limited to athletes. Tendinopathic changes are often observed in the older population which is part of the normal aging process. However, on the background of these changes, the threshold for how much load the tendon can withstand is lower, particularly if the individual lives a sedentary lifestyle. Hence what seems like a small amount of increased activity may be enough to irritate the tendon.
What are the signs & symptoms?
The most common sign of Achilles tendinopathy is posterior ankle pain and stiffness. This pain may be reproduced by squeezing the Achilles.
Pain when bending up the ankle (e.g walking up an incline).
Reduced strength or considerable tightness in your calf muscle.
Pain and stiffness may be more prominent at the beginning of exercise, ease off slightly once warmed up, and increase post activity once warmed down.
In a similar pattern, pain and stiffness may be more prominent first thing in the morning and before going to bed at night.
How can Physiotherapy help?
The initial phase of treatment aims to reduce the irritability of the tendon.
This may involve a combination of:
- Resting from the aggravating activity or reducing the frequency and load
- Icing post exercise
- Soft tissue massage
- Rigid taping
- Dry needling
- Joint mobilisation
- Activity modification/load management
Once the tendon becomes less irritable, the most effect way to heal tendons is to progressively load them with resistance-based exercises. Tendons love exercise! With the write type and dosage from your Physiotherapist, we can promote healing and advantageous adaptations to strengthen tendons as well as instant pain relief.
Your Physiotherapist will also undertake a thorough biomechanical assessment with you to find specific causes which may have placed you at greater risk of developing a tendinopathy in the first place.
Examples of this include:
- Current Loading Patterns
- Foot posture
- Reduction in optimal lower limb biomechanics
- Lack of ankle or foot joint mobility
- Reduced calf strength/endurance
- Increased calf tightness
